What is Periodontal (Gum) Disease?
Periodontal disease, also called “gum disease,” is the condition where infected gum tissue detaches from the tooth and is followed by loss of bone support around the tooth root. Deep pockets begin to develop under the gum surfaces, allowing bacteria to harbor and complicate the condition even more. If care is not taken, teeth will become mobile or fall out completely. In fact, it’s periodontal disease, not tooth decay, which is the leading cause of tooth loss in American adults.
1 Active periodontal disease is also closely linked with systemic health conditions like:
- Diabetes
- Heart Disease
- Respiratory Diseases
Other diseases that may be associated with periodontal disease include:
- Stroke
- Premature labor
- Small birth weight infants
- Osteoporosis
- Erectile dysfunction
- Obesity
Causes of Gum Disease
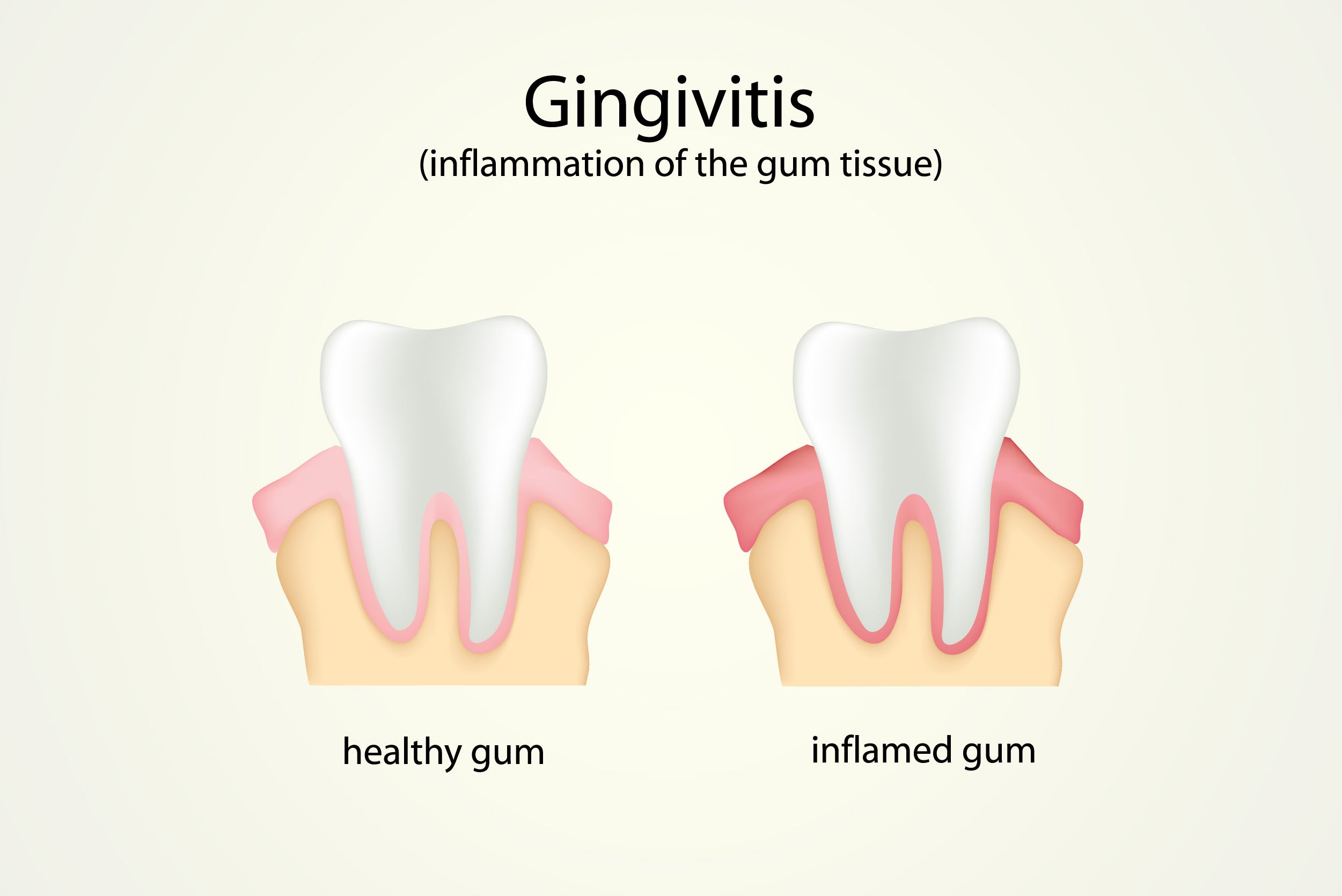
Gingivitis is the initial inflammation of the gum tissues along the margins of the teeth. The gums appear irritated, red, swollen, and may bleed during brushing or flossing. Thankfully, gingivitis is completely reversible as it is just the inflammation of gum tissue due to presence of plaque bacteria.
Periodontitis is progressed gingivitis that has extended inflammation into more areas surrounding the tooth. 3 Left untreated, periodontitis begins to lead to periodontal disease, as gum tissues detach from the tooth surface and bone levels around the tooth begin to recede.
Symptoms of Gum Disease
Gum disease has several symptoms that may or may not be evident to people that suffer from the condition. The most common symptoms that occur include:
- Bad Breath – The bacteria that cause periodontal disease can create a very odorous condition in the mouth; one that cannot be reversed with traditional home care methods. Halitosis associated with gum disease can be reversed only by the removal of this disease causing bacteria from the deep pockets.
- A Bad Taste – Some people experience a bad taste in their mouth, or can pinpoint what tooth the bad taste is coming from. This is due to aggressive, active infection.
- Red, Inflamed Gum Tissue – Tissue redness is a sign of inflammation and is due to an increased blood supply in the area. This is due to the body’s immune system targeting the area of infection with antibodies in the bloodstream. Normal, healthy tissues should appear smooth, coral in color, and pointed between the teeth. Puffy, rolled areas around the teeth are a clue that there is bacteria in the area.
- Bleeding Gums – If your mouth is healthy, you will not experience bleeding when you brush or floss. However, people with active gum disease will almost always report bleeding associated with their normal oral hygiene routine. What most people don’t know though is that if you brush and floss properly, normal gingivitis symptoms will reverse themselves within 2 weeks. Continued bleeding is an indicator that something more serious is going on.
- Tooth Mobility – One of the most serious complications of periodontal disease is tooth mobility, which ultimately leads to tooth loss. Mobility is due to the tissues around the tooth losing their attachment, and the bone support around the tooth being lost. While tissue re-attachment can be achieved, bone will not re-form on its own.
- Pain During Chewing – Associated with mobility, teeth with periodontal disease can become sore during meals, when pressure is applied to them. This is due to inflammation of the few ligaments and tissue still remaining around the tooth.
- Visible Tartar Buildup – Heavy areas of tartar buildup aren’t just unsightly they also house the bacteria that cause gum disease. Tartar is simply plaque bacteria that have calcified onto the tooth and the root surface. Without removing the tartar, the area of infection cannot be treated.
- Gum Recession and Sensitivity – Due to the detachment of healthy gum tissue, the gum levels can begin to creep down the roots, causing recession. This causes the teeth to appear longer, allows food to become trapped between them, and can predispose the root surfaces to sensitivity since they are not designed to be exposed to external elements.
Risk Factors of Gum Disease
There are several conditions that can predispose a person to gum disease and increase the rate at which their periodontal disease worsens. Knowing what these risk factors are can help patients manage their symptoms better and offer a holistic approach to treating their disease.
Smoking - Tobacco use is one of the most serious risk factors for patients with gum disease. Many times, smoking causes blood vessels to atrophy, preventing any type of healing from taking place, and also hiding normal underlying symptoms of the condition. People that smoke may never realize they are losing bone and gum attachment until their dentist checks for it. It can also make patients that smoke less likely to respond to treatment.
Diabetes - Blood sugar levels can affect the inflammation and infection of periodontal disease. Patients with unmanaged blood sugar often have more severe gum disease, and vice versa.
Family History - If your mother or father suffered from gum disease or lost their teeth prematurely, then their genetic susceptibility and oral bacteria were most likely passed on to you as a child. Thankfully, good oral hygiene can help counteract these factors, but neglecting your oral care will only allow a family history of gum disease an excuse to also occur in your own mouth.
Age - We naturally lose some bone support as we age. Combined with an active infection, bone loss can become more accelerated.
Hormones - Some women, although not all of them, suffer from inflamed, irritated gum tissue during pregnancy, menopause, or PMS. The fluctuating hormone levels can create false symptoms of inflammation and bleeding, even when bacterial levels are low.
External Factors - Stress can affect your immune system and make it more difficult to fight of diseases. Many people grind their teeth when they are experiencing stress, which places strain on the supporting tissues around the tooth.
Treatment for Gum Disease
Non-Surgical
- Deep Cleanings (Periodontal Scaling and Root Planing) - The most effective, non-surgical method to treat gum disease is removing the bacteria that are causing the disease. This is done through a professional dental cleaning where tartar and plaque are removed from the surfaces of the roots and below the gumlines. Normal brushing and flossing cannot access the deep pockets below the gumlines and will not reverse active periodontal disease.
- Medications - Topical medications (Chlorhexidine), locally delivered antibiotics (Arestin), or systemic antibiotics may be needed when a gum infection is severe. These can only be used for a short period of time, to prevent drug resistance and stain on the teeth.
Surgical
For very advanced stages of gum disease, a surgical treatment option may be needed:
- Flap Surgery - This procedure is performed by a periodontal specialist and involves the retraction of the tissue so that every area of the root surface can be cleaned. The tissue is then sutured back in place.
- Crown Lengthening - Removing diseased tissue in areas of very deep pockets will shorten the depth of the pocket, make it easier for the patient to access, and clean the area every day, preventing relapse.
- Bone Graft - Donor bone that is placed into the jaw can help offer additional stability in areas where tooth loss is a concern.
- Tissue Graft - If there is not enough healthy gum tissue around the tooth, and severe recession has occurred, then donor tissue can be placed over the area of the root. This protects it from sensitivity and adds additional tissue support.
- Proper Brushing - Angling your toothbrush toward the gumlines helps target and remove bacteria where it matters the most. Be sure to choose a high-quality toothbrush with gentle bristles that are soft on your delicate gum tissue. Brush at least twice each day for two minutes each time.
- Flossing - Wrap the floss around your teeth and Slide up and down under the gumlines, along the root of your teeth. If dexterity or access is a problem, try using a floss pick or water flosser. No matter how good you brush, you’ll never be able to remove bacteria under the gums without flossing. Floss at least once a day to remove debris from under the gums, between the teeth, where a brush won’t reach.
- Oralucent Toothbrush - The Oralucent toothbrush produces visible blue light that, importantly, is completely safe for humans but still kills harmful bacteria on contact. Daily use of the Oralucent toothbrush selectively suppresses bacteria commonly associated with destructive gum disease. Oralucent's advanced toothbrush actively kills the bacteria that form plaque and kills bacteria in places a conventional brush does not reach such as in gum pockets, on the tongue, and on the roof and walls of the mouth.
- Improving Your Immunity - A diet rich in key vitamins and fresh vegetables can improve your immune system and reduce infection in the body. DHA, vitamin C, iron, and fibrous fruit are all shown to increase blood supply, boost immunity, and speed up healing.
- Discontinue Using Tobacco Products - If you’re suffering from gum disease, smoking is one of the worst things you can do for your mouth. It is rare to see any type of healing take place in the mouth of people who smoke. Another great reason to kick the habit!
- Seeing Your Dentist for Routine Preventive Care - Regular prophylactic cleanings will remove tartar buildup, any areas of plaque that are missed, and help you keep your mouth healthy all year long. For patients with healthy mouths, professional cleanings are recommended every 6 months. People with active gum disease may need to be seen every 3 to 4 months until symptoms are reversed.